September is recognized as the national month for suicide prevention, a time to address the various factors contributing to suicide risks. One of the most overlooked and deadly intersections is the link between eating disorders and suicide within military populations.
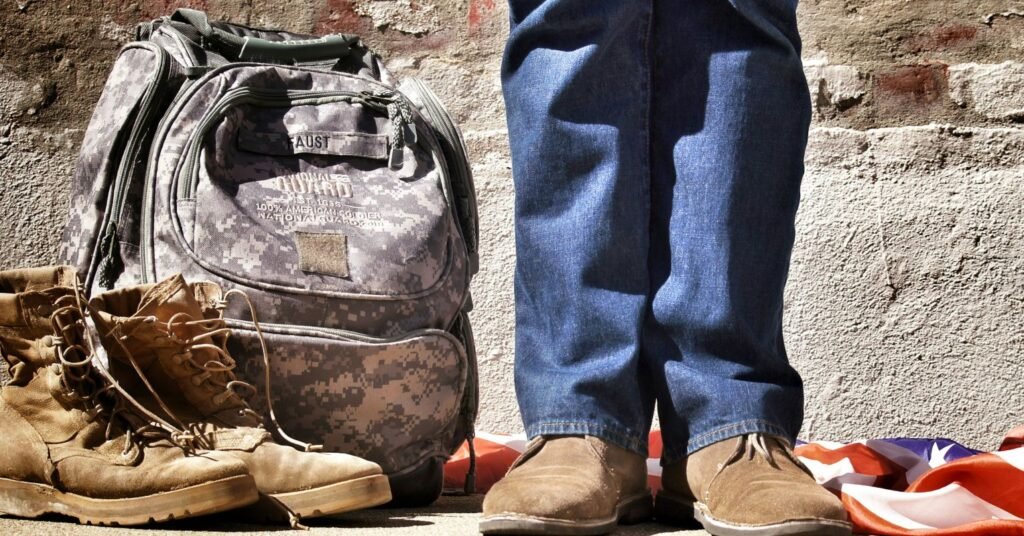
When we think of military service, we often envision strength, resilience, and unwavering discipline. However, beneath this facade lies a silent crisis. Eating disorders and suicide risks intersect in ways that are often ignored, causing service members and veterans to suffer in silence.
Eating disorders are not just passing phases or personal choices; they are severe psychiatric illnesses with some of the highest mortality rates among mental disorders. Anorexia Nervosa, for example, has one of the highest death rates among mental illnesses, with suicide being a significant cause of death. Other diagnoses, such as bulimia nervosa and other specified feeding or eating disorders (OSFED), also carry an increased risk of suicide compared to the general population. In the United States, approximately 10,200 deaths occur each year due to eating disorders, highlighting the severity of these conditions.
The prevalence of eating disorders in military and veteran populations is striking, with studies showing that a significant percentage of both female and male veterans exhibit signs of likely eating disorders. Moreover, a considerable number of individuals with eating disorders have attempted suicide, underscoring the emotional and psychological toll of these diseases. Despite these alarming statistics, eating disorders are often underdiagnosed and undertreated, making awareness, early identification, and intervention crucial, especially in populations where stigma and systemic pressures can mask warning signs.
Military culture, with its emphasis on dedication, discipline, and control, unintentionally contributes to the development of eating disorders and increases the risk of suicide among service members. Strict diets, intense physical training, and the pursuit of perfection can lead to disordered eating behaviors and negative body image issues. Additionally, the pressure to meet weight and performance standards, often enforced through measures like the “tape test,” can result in extreme behaviors such as crash diets and dehydration. Psychological factors, trauma-related experiences, and the presence of conditions like PTSD, anxiety, and depression further exacerbate the risk of both eating disorders and suicide within military populations.
The culture of silence within the military community can be particularly dangerous, as service members and veterans may fear judgment, stigma, or repercussions for seeking help. This silence perpetuates isolation, delays intervention, and strengthens suicidal ideation. By fostering open, stigma-free conversations, promoting early recognition, and providing compassionate care, we can effectively address the intersection of eating disorders and suicide in military populations.
As we observe National Suicide Prevention Month, it is crucial to shine a light on this hidden crisis. Eating disorders and suicide are not isolated issues; they are interconnected public health concerns that require attention and action. By recognizing warning signs, asking difficult questions, and creating supportive environments for help, we can protect those who have dedicated their lives to serving and protecting others.
If you or someone you know is in crisis or experiencing thoughts of suicide, seek immediate help by contacting the 988 Suicide & Crisis Lifeline or texting 741741 for the crisis text line. Remember, taking the time to ask, listen, and respond can make a life-changing difference. Let’s work together to raise awareness, break the silence, and support those who have sacrificed so much for our safety and well-being.